- What is nuclear medicine?
- What are radioactive tracers and radiopharmaceuticals?
- What is Single Photon Emission Computed Tomography (SPECT)?
- What is Positron Emission Tomography (PET)?
- What are nuclear medicine scans used for?
- What is nuclear medicine therapy or radiotheranostics?
- Are there risks?
- How are NIBIB-funded researchers advancing nuclear medicine?
What is nuclear medicine?
Nuclear medicine is a medical specialty that uses injected radioactive molecules to assess bodily functions and to diagnose and treat disease. Specially designed cameras allow doctors to track the paths and locations of these radiotracers/radiopharmaceuticals within living organisms. Single Photon Emission Computed Tomography or SPECT and Positron Emission Tomography or PET scans are the two most common imaging modalities in nuclear medicine.
What are radioactive tracers and radiopharmaceuticals?
Radioactive tracers are made up of carrier molecules that are bonded tightly to a radioactive atom. These carrier molecules vary greatly depending on the purpose of the scan. Some tracers utilize carriers that interact with a specific biomolecule in the body and can even employ the patient’s own cells. For example, in cases where doctors need to know the exact source of intestinal bleeding, they may add radioactive atoms to, or radiolabel, a sample of red blood cells obtained from the patient. They then reinject the radiolabeled blood, which would emit a type of light known as gamma radiation. With gamma camera detectors, doctors can follow the path of the blood in the patient. Any accumulation of radioactivity in the intestines informs doctors of where the problem lies.
FDA-approved radioactive tracers, called radiopharmaceuticals, meet FDA’s exacting standards for safety and appropriate performance for the approved clinical use. The nuclear medicine physician will select the radiopharmaceutical that will provide the most specific and reliable information for a patient’s particular problem. The radiopharmaceutical that is used determines whether the patient receives a diagnostic SPECT or PET scan.
For most diagnostic and therapeutic studies in nuclear medicine, radiopharmaceuticals are administered to a patient by intravenous injection. However, a radiopharmaceutical may also be administered by inhalation, oral ingestion, or direct injection into an organ or local region. The mode of radiopharmaceutical administration will depend on the disease process that is to be studied.
What is Single Photon Emission Computed Tomography (SPECT)?
SPECT imaging instruments provide three-dimensional (tomographic) images of the distribution of individual molecules of radiopharmaceuticals or other radioactive tracers that have been introduced into the patient’s body. SPECT imagers have gamma camera detectors that can detect gamma rays emitted from the compounds that have been injected into the patient. The cameras are mounted on a rotating gantry that allows the detectors to be moved in a tight circle around a patient who is lying motionless on a bed. Once a large number of 2D projection images are recorded at different angles around the body, a computer uses this information to construct a 3D image.
What is Positron Emission Tomography (PET)?
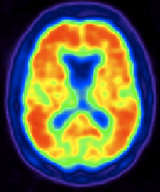
PET imaging instruments also use radiopharmaceuticals or other radioactive tracers to create 3D images. The main difference between SPECT and PET scans is the type of radioactivity used. While SPECT scans can measure a large variety of gamma rays, the decay of the radiolabels used with PET scans produces small particles called positrons — particles with the same mass as electrons but oppositely charged. When positrons react with electrons in the body, the two particles combine and annihilate each other, producing a small amount of energy in the form of two coincident gamma ray photons that shoot off in opposite directions. The photons’ energies are identical regardless of the type of positron-emitting radionuclide that is used. The detectors in the PET scanner measure these photons and use this information to create images of internal functional molecular processes.
What are nuclear medicine scans used for?
SPECT scans with specific radiopharmaceuticals are primarily used to diagnose and track the progression of heart disease, such as blocked coronary arteries. There are different radiopharmaceuticals to detect disorders in bone, gall bladder disease and intestinal bleeding, etc. SPECT agents have recently become available for aiding in the diagnosis of Parkinson’s disease in the brain and distinguishing this malady from other anatomically related movement disorders and dementias.
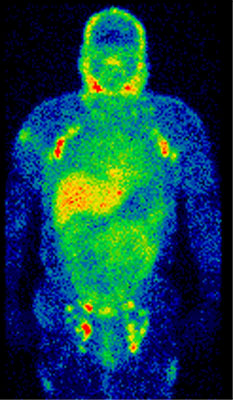
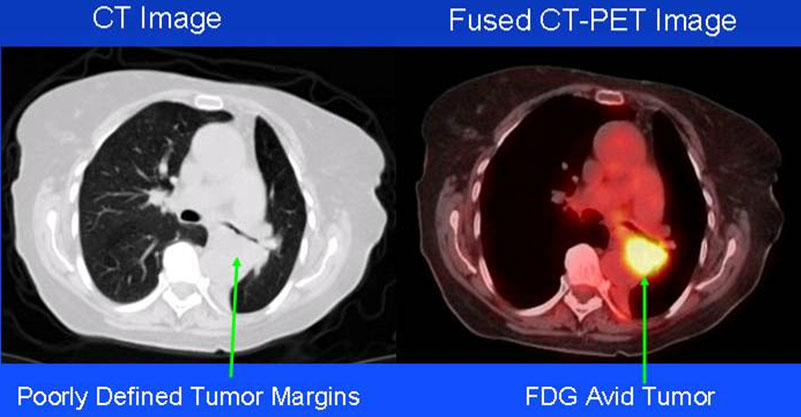
The major purpose of PET scans is to detect cancer and monitor its progression, response to treatment, and to detect metastases. It is also being utilized more frequently for diagnostic brain and cardiac imaging. The utilization of glucose, a form of sugar, depends on the intensity of cellular and tissue activity, so it is greatly increased in rapidly dividing cancer cells. In fact, the degree of aggressiveness for most cancers is roughly paralleled by their rate of glucose utilization. In the last 15 years, slightly modified radiolabeled glucose molecules (F-18 labeled deoxyglucose (fluorodeoxyglucose) or FDG) have been shown to be the most general and best available radiopharmaceutical for detecting cancer and its metastatic spread in the body.
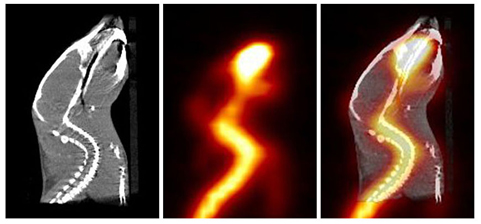
A combination instrument that acquires both PET and CT scans of the same body regions in one examination (PET/CT scanner) has become the primary imaging tool for the staging of most cancers worldwide. Fused PET/CT scans more clearly show tumors and are therefore often used to diagnose and monitor the growth of cancerous tumors and their response to various therapies.
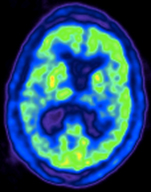
Recently, a PET radiopharmaceutical was approved by the FDA to aid in the accurate diagnosis of Alzheimer’s disease, which previously could be diagnosed with accuracy only after a patient’s death. In the absence of this PET imaging test, Alzheimer’s disease can be difficult to distinguish from vascular dementia or other forms of dementia that affect older people.
What is nuclear medicine therapy or radiotheranostics?
In addition to their diagnostic applications, radiopharmaceuticals are also used in therapeutic studies or procedures in a similar manner to how non-radioactively labeled pharmaceuticals are used to treat a wide range of conditions from headaches to cancer. A very small dose of a particular radiopharmaceutical is first injected and diagnostically imaged by the SPECT or PET cameras. If doctors determine that the uptake of that radiopharmaceutical is appropriate, then the patient will be injected with a considerably larger quantity of that radiopharmaceutical or its radiotheranostic pair so that the radioactivity bound to it can provide therapy for the patient’s medical condition. A radiotheranostic pair is almost exactly the same as the diagnostic molecule except for the type of radioactive atom bound to it (e.g. some release x-rays or gamma rays useful in imaging, and beta or alpha particles more useful in therapy). In a process called dosimetry, a medical physicist may use available diagnostic images to calculate the radiation dose administered to and absorbed by organs in the body. After treatment, further diagnostic imaging can help determine how a patient is responding to the therapy.
Are there risks?
The total radiation dose conferred to patients by the majority of radiopharmaceuticals used in most diagnostic nuclear medicine studies is no more than what is conferred during routine chest x-rays or CT exams. There are legitimate concerns about possible cancer induction even by low levels of radiation exposure from cumulative medical imaging examinations, but this risk is accepted to be quite small in contrast to the expected benefit derived from a medically needed diagnostic imaging study. Note that radiotheranostic procedures intentionally introduce larger doses of targeted radiopharmaceuticals to regions of concern in order to combat the disease or condition.
Like radiologists, nuclear medicine physicians are strongly committed to keeping radiation exposure to patients as low as possible, giving the least amount of radiopharmaceutical needed to provide a diagnostically useful examination.
How are NIBIB-funded researchers advancing nuclear medicine?
Research in nuclear medicine involves developing new, more specifically targeted radiotracers for both diagnostic and therapeutic procedures, as well as developing technologies that will help physicians produce clearer pictures using less overall radiation or acquire the images faster. NIBIB funds many of these newest developments.
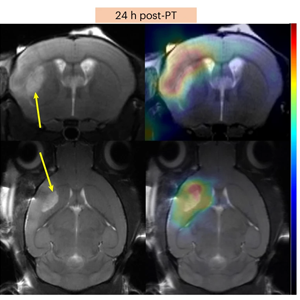
Probing the early signs of neurological disease
Neurodegenerative diseases, such as Alzheimer’s and amyotrophic lateral sclerosis (ALS), are typically diagnosed once physical symptoms have manifested, but by then, it may be too late for treatment to be effective. To catch these diseases earlier on, researchers at St. Jude Children’s Research Hospital and the University of Virginia have developed an antioxidant-based PET probe that can be used to detect oxidative stress, a damaging phenomenon that plays a key role in neurodegeneration. The team deployed their approach in mouse models of chronic and acute neurodegeneration, successfully quantifying oxidative stress, and suggested that the technique could one day be useful for evaluating experimental early interventions.
Reviewed September 2025
