Communities also play featured role as curtain rises on testing
COVID-19 test developers have bioengineered a wide array of new diagnostic technologies – with varied configurations and attributes that set each apart. Some of the tests that provide rapid results differ by the following:
- types of sample to be collected for testing (nasal, oral, saliva, or blood),
- processes for obtaining results (in a lab, or on a cartridge or test strip at the point of care),
- duration (minutes, hours, or days to get results), and
- methods of detection (in the channels of a microfluidic chip, or with an optical spectrum reaction, or by a patented chemical formula).

While each test is impressive in its cutting-edge innovation, they must all perform to regulatory standards for test accuracy, usability, and acceptability by the end user.
To assess these variables, many of the diagnostic tests introduced through the NIH Rapid Acceleration of Diagnostics (RADxSM) initiative will be studied by the COVID 19 Test Us clinical studies program, a resource established by the RADxSM Clinical Studies Core. COVID-19 Test Us is supported through federal stimulus funding from Congress to the NIH with a portion going to the Heart, Lung, and Blood Institute (NHLBI) for clinical studies that are part of RADxSM.
The COVID-19 Test Us program was conceived soon after the RADxSM launch in April to facilitate clinical studies for testing technologies in the real-word setting. Clinical studies are necessary to demonstrate that tests perform as proposed, both to the satisfaction of the person administering the test—often a clinician—and to that of the person being tested. Another important aspect of the tests being evaluated is the test performance, whether the novel test has comparable sensitivity and specificity to that of current FDA-authorized tests.
During a public health emergency such as the COVID-19 pandemic, the U.S. Food and Drug Administration (FDA) may allow the emergency use of not fully approved medical products, or unapproved uses of approved medical products, to diagnose, treat, or prevent serious or life-threatening diseases such as during the pandemic. Medical device manufacturers—such as diagnostic test developers whose technologies have been advanced by RADxSM—seek Emergency Use Authorization (EUA) for their diagnostic and screening devices. To make a case for this special use, they must present data about their tests to the FDA after the technology is evaluated through RADxSM Tech.
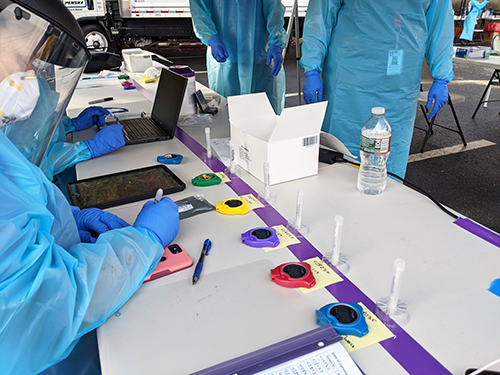
“Each COVID-19 Test Us clinical study is designed differently, to account for the type of test, supplies required, modes of implementation, and unique methods for displaying readouts,” said Erin Iturriaga, D.N.P., a program officer at the NIH Heart, Lung, and Blood Institute, whose expertise is in clinical trials management, education, and regulatory responsibilities. She is among the numerous specialists throughout NIH who have assumed important roles in RADxSM, pivoting her focus to address the COVID-19 pandemic. “Researchers working with COVID-19 Test Us collect the study data that is subsequently used by the test developer to obtain EUA for an initial type of use case or for an expanded use case than its original EUA. Our researchers pride themselves in being nimble enough to adapt to the diversity of tests.”
The COVID-19 Test Us study team provides knowledge of FDA requirements when a device developer is seeking an EUA. Developers typically must submit data as part of meeting EUA requirements based on how a test is intended to be used, whether, for instance, in a school, a nursing home, or workplace. The FDA also expects to receive data that represents how the test performs with various age groups, including children and older adults, and from a balance between men and women, and an otherwise diverse population. The team designs studies not only for the first conceived use of a test, but for expanded or amended EUA, such as when an already approved test is proposed for use with a sample type—whether saliva, nasal, or blood—that is different from the original EUA.
“COVID-19 Test Us study-design experts sit down with a representative from the company to talk through their goals for the testing study,” said Jue Chen, Ph.D., NHLBI program officer who also has been working with RADxSM Tech, adding that the Clinical Studies Core team and the company are represented in this discussion by their respective regulatory experts. “Data is captured for the company to use in its application for an initial EUA or amended EUA.” Together, they design a study that measures diagnostic test usability and acceptability, and the accuracy of the test. During the clinical study, both the person administering the diagnostic test and the person being tested respond to a questionnaire.
All de-identified data collected by the COVID-19 Test Us program is deposited in a HIPPA- and FDA-compliant server, called the COVID-19 NIH Data Hub, for data sharing. This secure, cloud-based research hub may facilitate machine learning along with other COVID-19 data. “Besides age group and ethnicity, we also collect elements of data, such as whether a participant is a smoker or vapes,” Iturriaga said. “Even before we were asked, we knew these would be important pieces of information to collect for future research purposes.”
COVID-19 Test Us works with a Community Health Engagement team in recruiting participants for studies and creating public awareness. Recruitment occurs variously at community outreach events, nursing homes, schools, and by invitation to people scheduled for medical procedures. Participation is currently limited to those residing in the vicinity of partner institutions, which are in central Massachusetts (University of Massachusetts Medical School), metropolitan Atlanta (Emory University), east Baltimore (Johns Hopkins University), and Evanston, Illinois (Northwestern University). Future clinical studies may involve more locations and even at-home testing.
The COVID-19 Test Us website, covid19testus.org, provides information about clinical study research for potential participants in COVID-19 testing studies. Participants may also learn of opportunities to join a study from public service announcements that air on local radio stations. The program includes a pediatric component for studies that include children, called COVID-19 Test Us Kids.
Test developers, COVID-19 Test Us study design experts, and participants from the community all have essential roles to play in the rapid deployment of COVID-19 tests that will help the nation in the return to school and work.
